Dr. William Lowery, a practicing pulmonologist at Alameda Hospital in Northern California, was diagnosed with Limb-Girdle muscular dystrophy some 20 years ago. He’s now founded a non-profit organization to help others shorten their diagnostic odyssey with free genetic testing and his expert guidance.
Below are un-edited portions of the interview with Dr. Lowery:
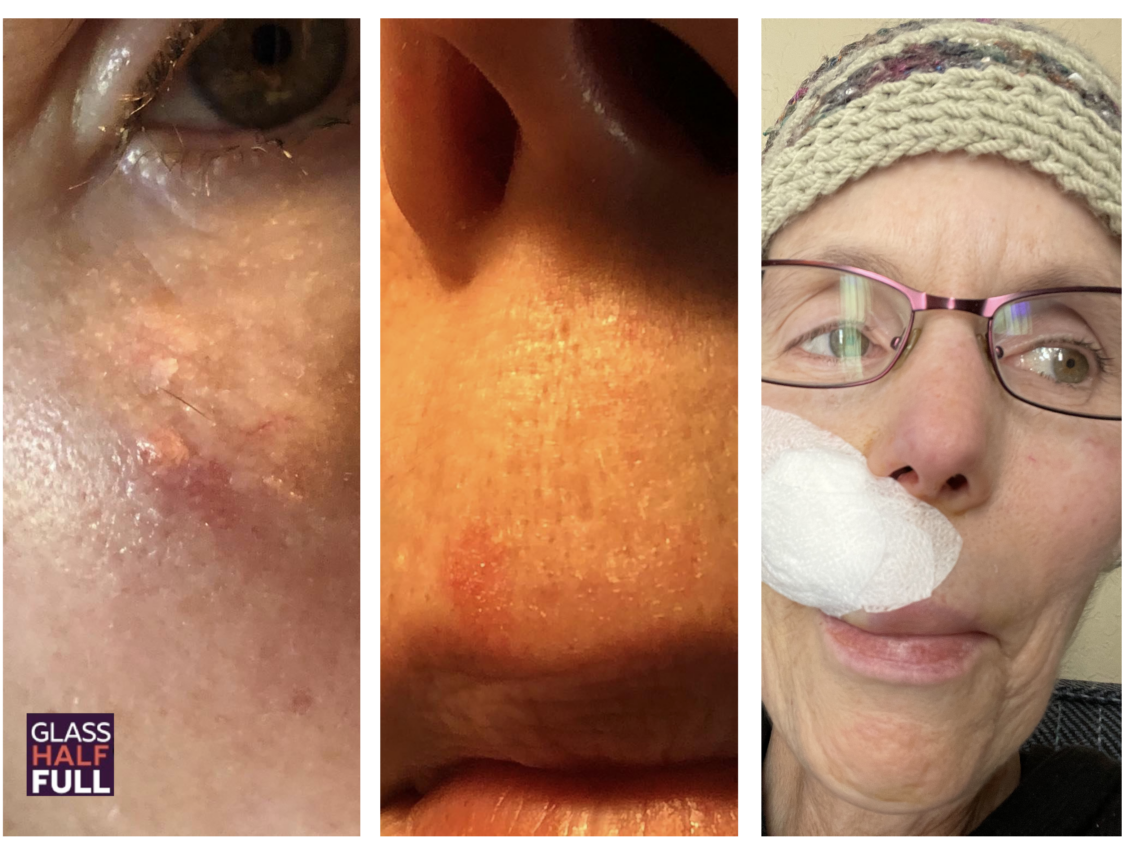
I was biopsied at Duke University because actually ten years prior to that, my mom had rounded up. My dad had the same condition, a limb girdle muscular dystrophy. His dad had it. And as far as we knew at the time, I was the only one of five children that that showed any sort of weakness. And so my mom somehow got in touch with Duke University and rounded up all these relatives in the Lowry Family Tree, who had this late onset limb girdle muscular dystrophy. And then so Duke said, Look, we need a muscle biopsy. Will somebody come forth? And so I flew from California to Durham, North Carolina, and had a left leg muscle left leg muscle biopsy. And there they found that it was an inclusion body myopathy. So that was kind of an unusual that was kind of a red flag for a muscular dystrophy because there’s several types of inclusion body. But it they finally got together with a finish, a group of Finnish researchers and Italian researchers who had families with the same sort of inclusion bodies. And together they found that it was a gene variant on the the DNA Jbe six mutation. It’s on chromosome seven. I forgot where it is and that, but they were able to put that on the map, and that was probably back in two thousand five. And since then, there’s been a genetic explosion in being able to arrive at a genetic diagnosis. And maybe, you know, you wouldn’t need a muscle biopsy if you had the genetic diagnosis. So basically, I would say probably 2001 with my biopsy, I knew I had an inclusion by a muscular dystrophy inclusion body of myopathy they call it, but it probably wasn’t genetically defined until 2005 or 2007.
As a as a child, I could see my dad getting weaker and weaker and not being able to do things. And the same with my grandfather and my grandfather, his family, you know, relatives had and they just way back then around the eighteen hundreds, you were just lazy. You know, he he had an accident. He claims he had an accident when he was plowing and a plow fell on him. And that’s what caused his weakness in his legs. So as a farming injury? Hmm. And then my dad sort of knew that something was up, but he never went to the doctor. And when he finally went to the doctor and found out he had a muscular dystrophy and it was incurable, you know, he it really upset him. I thought there was a pill he could take or surgery. And so my mom, you know, I guess, saw me getting a little weak or whatever, and actually, to her credit, really did all the legwork on getting all the relatives. You know, there’s a family reunion, I think, which kind of triggered all this. And she just put all these people together with Duke University and and the rest is kind of history. I knew. So I saw my dad, but you know, I was still running doing everything I wanted to do.
But the thing about me is that I was I always came in last in red and foot races and I was picked last for kickball team. And you know, I mean, so but it never, never dawned on me that there was something wrong with me. I was just happy to be involved. And, you know, I had the usual desires and drives as a teenager and I wanted to play professional basketball. You know, that was never to be, of course, but I never put two and two together. I ran Cross Country in college. I was still, you know, I did fairly well. And you know, I was, you know, I was doing everything a person could do. It’s just that I wasn’t the fastest person in the world. But again, it wasn’t until I was like 30 or 30 that I started putting things together. You know, this was past my medical training, and I still thought I was normal. But maybe, maybe I don’t know why. I guess you would call it denial, but it was on a very subconscious level.
And it was again, it was almost a selfish desire to go into medicine because, you know, I majored in a bachelor’s in science, chemistry biology and I said, you know, I thought, What am I going to do with all this? And I’m kind of a social guy. And so I thought medicine was a nice blend of that. I guess I should have taken over my dad’s business. He was an engineer at a metal working shop, but it just didn’t interest me at all. So I chose my own path, you might say. But then, you know, through medical school, I sort of had an awakening that, you know, there’s something to this. Maybe I could help this out. But you know, all the research was still primitive, and I got drawn into other areas internal medicine and then pulmonary, which I’m a practicing pulmonologist now. Thirty five years at the same hospital in Alameda.
there is a new naming, a new naming system I think about five years ago where you know of the the types we know that, you know, I kind of like to split things into autosomal dominant world, right? I’m a recessive now. Myotonic, of course, is autosomal dominant. As I recall, two types. Yeah, so. So sticking with the autosomal dominant, they tend to be milder later onset and with exceptions, obviously, and some can involve heart and lungs more than others versus autosomal recessive, which are 80 percent of the muscular dystrophy, the limb girdle muscular dystrophy. We’re not talking about Duchenne. That’s kind of in a different category, better research and stuff like that. So the autosomal recessive that is the two bad genes, they tend to be younger onset involve cardiac and respiratory a lot more frequently. So, you know, I am thankful in a way that I had a later onset. Having said that, there are there are genetic engineering company Sarepta in particular that’s come out with whether they’re developing therapy for five autosomal recessive limb girdle muscular deficiencies to A, B, C, D and I think I or something like that. So you know, that can be easily googled by just Googling Sarepta, but so they’re about five years ahead of autosomal dominant as far as therapy.
So that’s the way I look at the world, and that’s why I developed a foundation the LGM de 1B Foundation, which doubles as an autosomal dominant registry. And so anybody who has an autosomal dominant condition, even yourself, if you’re not part of a foundation and you know, I mean, it’s like the 20 percent we’re really like stepchildren, you know, so I felt compelled to organize the autosomal dominance because in our world, the therapy will be different. But but homogenous the same things that would help you would help me versus like CRISPR, antisense oligonucleotides knock knock down strategies that will block the bad protein. So that’s a couple of years away. But that’s why I thought I would organize people in my registry. So when people come knocking say, Look, do you have Mathebula myopathy at this time? Do you have myotonic dystrophy at this time? You know, if you’re not already involved in that sort of registry that might represent you, then I’ll take all comers, all stragglers, so to speak.
Well, you know, all you know, University of Washington, St. Louis is the epicenter for SGMD 1d, the DNA JB six variant. So we kind of hooked our way. Into to them, and it just so happens that one of the main researchers has the same condition, so he’s highly motivated to find a cure. So anyway, there are other there are seven other centers who are in this consortium that are also looking into that as well. But they’re the main folks. But again, they were going to enroll two or three people a month and a natural history study, but that came to a screeching halt. So what do you do in the meantime? Lo and behold, with social media, with the relaxation of of of of licenses across the United States, medical licenses, what I did was and I found out that there was a lot of free genetic testing. You know, like Invité has a lot of sponsored testing, not only for muscular dystrophy, but seizures for I mean, if you go to Invité and look at their sponsored panels, it’s voluminous. You can get a lot of free testing.
So I signed up with them and I I put the word out through social media that I would facilitate free testing. But you had to have a doctor who could review the test in the provides free genetic counseling. So everything was in place for me medical legally. I was just the conduit, but I was enjoying analyzing this and giving my two cents because like you, you’ve learned a lot about these conditions. And so I’m able because I had the condition, I have a medical license and I’ve gone to, you know, sort of grad school, you know, night school on muscular dystrophies and genetics. And I’ve watched a lot of YouTube channels, but I feel like I’m qualified enough to be at least a conduit. So as you know, I’ve got up to one hundred and thirty patients and about 30 percent I’ve made a diagnosis. It was not known. So I’ve helped, you know, a third of people. There’s other people that we have suspicious genes and we’re still kind of doing other things to try to sort their conditions out.
All the genetic testing that I just told you through Invité and other other big powerhouses is sponsored. And again, you know, genetic therapy companies want, you know, they make big money if they can deliver therapy. So it’s it’s good for them. I guess everybody’s making money. I don’t question it. I just I just go for it as long.
So that’s very gratifying. But, you know, the autosomal recessive, there are treatments for that and there. We’re going clinical trials now, and it’s very exciting, but again, autosomal recessive. Your audience has to understand that autosomal recessive is like having two bad cars in your garage. You can’t go anywhere. So all you have to do is slip in a car, a good car and you’re off to the races. Autosomal dominant is different because you autosomal dominant gene is producing a protein that’s toxic. Ok, so you know you can’t get rid of it. All you can do is go in with CRISPR and plug it out and put in a good gene. Or you can send in a little binding messenger RNA to block that bad art and messenger RNA called a knockdown strategy. So those are the two things that are working working right now for autosomal dominant and probably autosomal recessive, too. But all you have to do is slip in a good gene. And you know, the case I give is hemophilia. Ok, hemophilia is, you know, they bleed into their joints and bleed into their tissues, and they receive a million dollars worth of blood products a year. Wow. So, you know, and they don’t like, you know, they fall and they say, Oh my God, my joints are going to swell up and I’m going to be in pain for days.