People with anxiety, autism, blindness or low vision, deaf and hard of hearing, mobility challenges, chemical sensitivities, or PTSD may face unique challenges visiting a dental office. Now with the additional barrier — the COVID-19…
If you, or someone you know, has a muscle or nerve condition such as Multiple Sclerosis, Spinal Cord Injury, Amputation, Osteoarthritis, Parkinson’s Disease, or a neuromuscular disease (i.e. myotonic dystrophy, SMA, Charcot Marie Tooth, Becker’s,…
It’s April Fool’s Day so we’re mixing things up with an unhelpful advice rant. One can’t be positive 100% of the time. Now is the opportunity to share about all of the weird things people…
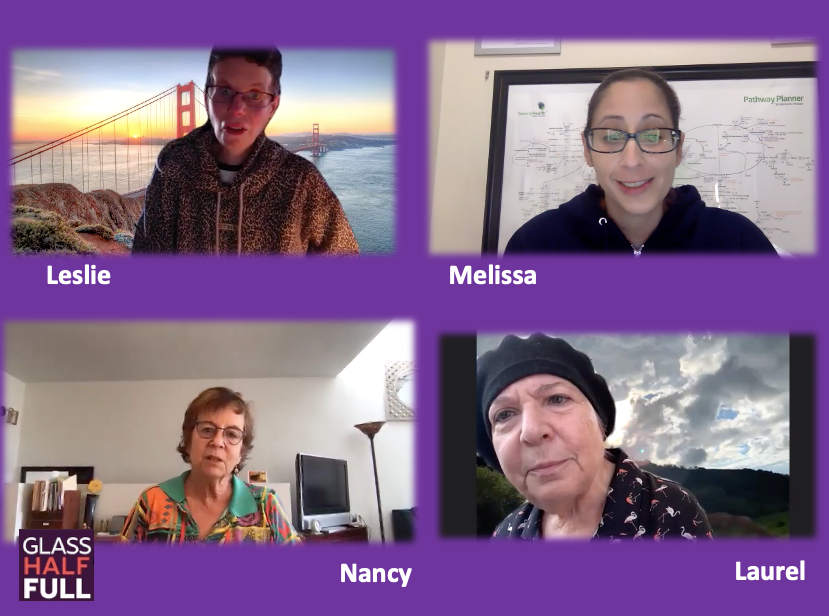
Being diagnosed with a chronic, debilitating disease can certainly bring stress to one’s life. In fact, that stress can be significant enough to be called trauma. How one handles this stress varies. Some people have…
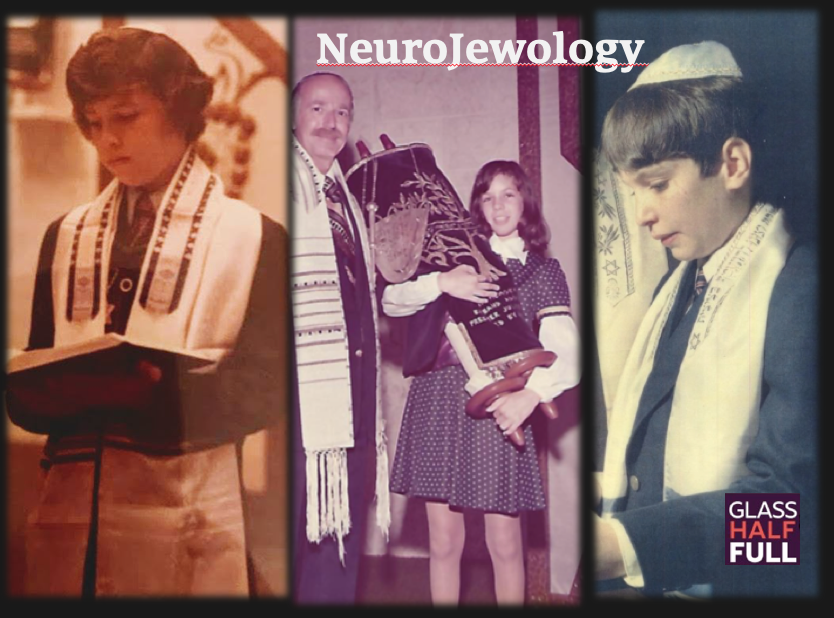
Two friends from grade school share their stories of a diagnosis of a neurological condition. Marc has Multiple Sclerosis and Steve has Parkinson’s disease. I have a form of muscular dystrophy called myotonic dystrophy. It’s…
Pilates: Core Strength, Alignment, Pain Relief, and Neural Reconnection
- October 6, 2019
- Tagged as: breath awareness, core muscles, exercise, Feldenkreis, foot drop, Franklin Method, hip, independence, mindfulness, movement therapy, myotonic dystrophy, neural connectivity, pain, Parkinson's disease, physical therapy, Pilates, proprioception, PTSD, scoliosis, trauma, yoga
Practicing Pilates can be done on a mat or with any number of devices such as the Reformer. Shannon Knorr, a yoga and Pilates instructor, talks about therapeutic Pilates to help with body alignment, pain…
Vocal problems can occur for people with all types of conditions — Parkinson’s disease, muscular dystrophy, stroke. Acute laryngitis is very common while chronic laryngitis affects over 20% of the population. Christine received a diagnosis…
A brand spanking new podcast episode will appear…hopefully before the end of the week. It will be Food = Medicine: Mushrooms. But, for now…check out these Food = Medicine podcast episodes: An interview with Sandor…
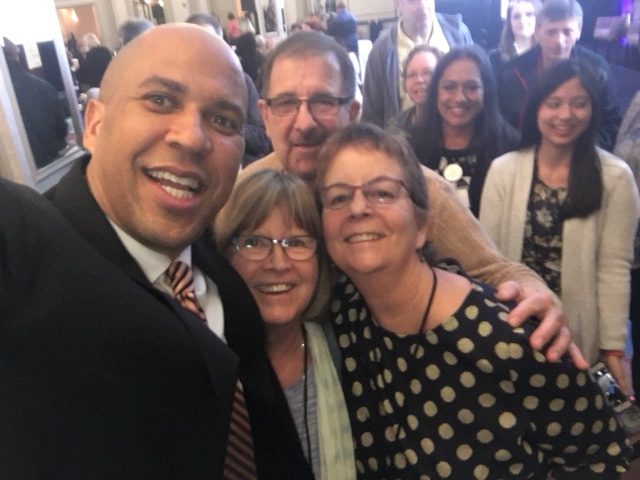
Maybe you have a firm grasp on what Patient Advocacy is all about? This episode explores different ways people with disabilities, their allies, and their caregivers practice advocacy. Whether you’re searching for the best healthcare options,…
In the continuing series, Food=Medicine, Cooking with Love explores different interpretations of how love can be a vital element in the food we eat. Whether it’s part of the mission of a local organic farm,…