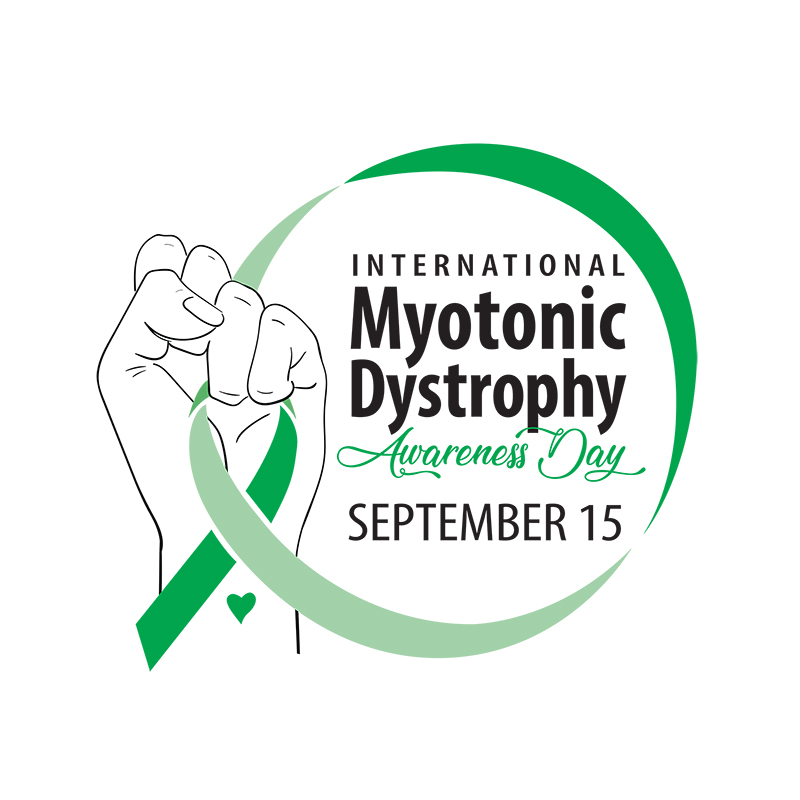
September 15th is International Myotonic Dystrophy Awareness Day. To learn more about helping educate and advocate for Myotonic Dystrophy visit the Muscular Dystrophy Association or Myotonic Dystrophy Foundation.
The purpose of International Myotonic Dystrophy Awareness Day is to garner the attention of the wider general public, policy makers, regulators, biopharmaceutical representatives, researchers, health care professionals, and anyone with an interest in changing the future of myotonic dystrophy. Raising awareness of myotonic dystrophy will help improve service provision, basic research, drug development, and policymaking related to the disease. Increased funding for myotonic dystrophy research will improve health outcomes, reduce disability, and increase life expectancy for individuals living with the disease, and holds great promise for helping individuals with diseases with similar genetic bases, such as Fragile X syndrome and Huntington’s disease.
To learn about the different types of myotonic dystrophy, visit this NORD webpage.
In addition to this podcast host/producer who lives with Myotonic Dystrophy Type 1, the following podcast episodes have featured guests living with DM1, DM2, or caregivers in a DM family:
Food = Medicine
Passion and Motivation to Move through the Hard Stuff
Working with Wounded Warriors
Music Gives Me a Peace Bubble
Salute to Caregivers
Stories of Healing with Essential Oils
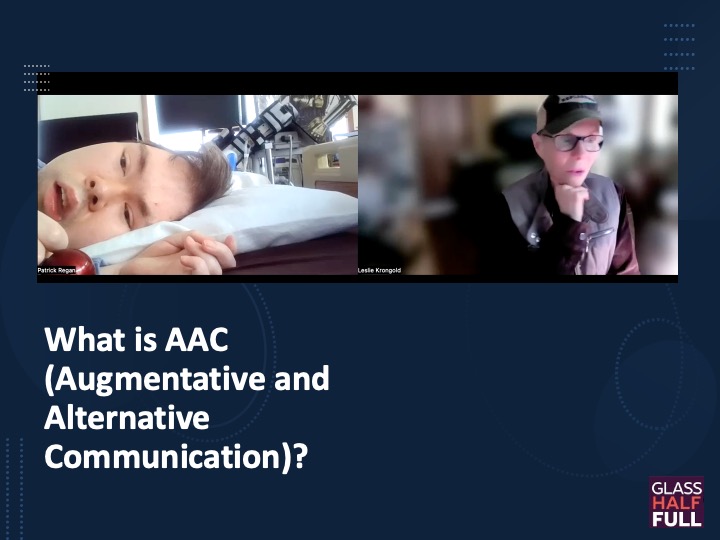
Transcript:
Welcome to my first ever complete podcast episode about my rare disease myotonic dystrophy. Or as we like to call it DM because that’s how it’s referred to in medical literature.
Now it’s not like it’s been a secret that I have this disease. I just haven’t spoken in detail about it unless it was relevant to the guest or topic of the podcast episode.
But I just went to San Diego to attend the first in-person patient conference we’ve had since the pandemic. For two years we held a virtual conference. And there I was reminded that September 15th is now considered International Myotonic Dystrophy Awareness Day.
I was also inspired to do an episode because the logo design for this day was created by a young Canadian woman whom I have now met in person – including her mother. check out the design by visiting the Glass Half Full website.
The purpose of this International Myotonic Dystrophy Awareness Day:
is to garner the attention of the wider general public, policy makers, regulators, biopharmaceutical representatives, researchers, health care professionals, and anyone with an interest in changing the future of myotonic dystrophy. Raising awareness of myotonic dystrophy will help improve service provision, basic research, drug development, and policymaking related to the disease. Increased funding for myotonic dystrophy research will improve health outcomes, reduce disability, and increase life expectancy for individuals living with the disease, and holds great promise for helping individuals with diseases with similar genetic bases, such as Fragile X syndrome and Huntington’s disease.
Along with Alexandra’s logo design, I’ve included links to two organizations that have additional information about the Global Alliance and how you can advocate for those with myotonic dystrophy.
Another reason I think I’ve felt inspired to draw attention to my rare condition is that it’s not so rare…anymore. At last week’s Patient Conference, I had the unusual and bittersweet opportunity to meet a young couple who are newly diagnosed because their infant – born 7 weeks ago – has congenital myotonic dystrophy. I was drawn to this woman who looked familiar and maybe familiar just means that her facial features resembled so many of us with DM Type 1 – thin face, sunken temples, pronounced cheek bones. We often look like we can be family. But I discovered it was her first time there due to her new diagnosis. Their baby was still in the NICU at a Bay Area Children’s Hospital. I acknowledged their sense of overwhelmedness and assured them they would meet many similar families to help them find their way through all of this.
A couple of hours later my partner texted me – from another conference session – that there were people there from Fort Bragg. Last year we moved to rural California. None of the medical professionals I’ve met here have known someone with myotonic dystrophy. I went to meet them – and sure enough – it was the young couple I’d met earlier. Now there will be three of us with myotonic dystrophy within 10-minutes of each other.
This family will have a lot of difficult issues to work through. Healthcare in this rural community is not like living in a metropolis. I have to drive 2-4 hours to see a pulmonologist, neurologist, or endocrinologist. The families I know of that have had congenital kids thrive the best have been able to provide all types of therapeutic modalities. Congenital kids often need major respiratory and GI help for the first few years. Developmentally many are on the autism spectrum and require special education and assistance.
As an adult with DM, I made the decision to opt for the more natural environment in lieu of the most modern medical technology but I doubt one would do that for their child.
So, I’ve talked a little about babies born with congenital DM. In the 20-something years since my diagnosis and involvement with two patient advocacy organizations I have heard, and known, many congenital kids who have died. If you know my story, I’m most certain that the sister I had for three days – in 1963 – also had the congenital form of the disease. Hardly anything was known about DM then and medical technology did not exist to help her live. But one thing I was able to do at the conference was introduce this couple to Richard whose son is…I believe 32 years old now…and has the congenital form. Hope is important in our lives.
In addition to adult-onset DM type 1 there is a middle-range category often referred to as juvenile onset DM type 1. These are children that are diagnosed sometime in their childhood, but they may have had some unusual issues at birth, like club feet. It seems to me that often their issues don’t lead to a diagnosis until something dramatic in their families occurs such as a congenital birth or sudden heart attack of a relative.
I’ve met so many families that thought their teen or young adult was just lazy and lacked motivation. There’s a whole track at these patient conferences for JOAs – juvenile onset adults. Many of these adults weren’t very successful in school and couldn’t hold down a job.
And often you can have all three in one family. The diagnosis occurs with the birth of a congenital baby. The mother has had what the family thought were personality issues. The grandparents end up caring for the congenital child. In their house are at least three people with myotonic dystrophy.
And then there is DM type 2. A good description of the symptoms for both DM types can be found on the NORD website: https://rarediseases.org/rare-diseases/dystrophy-myotonic/ but from what I currently know is that there are many similar symptoms but in general DM2 is less severe. There is no congenital form of DM2 nor does there seem to be a juvenile form. The people I know with DM2 don’t have the look that I mentioned earlier. Although last week I did notice a few of my DM2 friends have lost weight, i.e. muscle loss and are moving slower, like myself.
In the late 1990s a researcher known as Dr. Tee Ashizawa co-founded the International Myotonic Dystrophy Consortium (IDMC) to bring together scientists and clinicians focusing on DM. Every two years the meeting location changed and eventually began attracting patient families as well. I had the opportunity to attend two of those meetings – one in Wurzberg, Germany and the other in San Sebastian Spain.
Seeing people with myotonic dystrophy from other countries is pretty amazing; unfortunately, few spoke English and that’s the only language I’m fluent in. but in an online chat right before the IDMC met in Spain I became friendly with a man in Switzerland with DM1. Erich and I wrote emails back and forth and became close friends. I even convinced him to join Facebook. We met twice in person twice before he died; the first time in Barcelona and then in Iceland.
Erich was able to attend support group meetings in France, Germany, and Switzerland so I got to hear about patient’s stories from outside the U.S. At the IDMC I saw people who looked like me – thin with the similar facial features. I appreciated hearing presentations from different researchers – Japanese, Germans, Italians, Dutch. Some would include photos of their patients. Maybe other diseases have these global connections too? I hope so.
Myotonic dystrophy is known to be the most common adult-onset muscular dystrophy. Previously thought to affect 1 out of every 8,000 in the general popular, recent prevalence studies suggest that it is more common with 1 out of every 2,100 people. Since the condition is multi-systemic and the symptoms can be written off as something else – i.e. lack of motivation, Irritable bowel syndrome, weakness, or even MS….it is often un-diagnosed.
My partner and I often spot someone – a stranger – who resembles me and we wonder, “does that person have DM and not know it?” Drawing awareness and educating healthcare professionals is important.
At this year’s patient conference there were more pharmaceutical and biotech companies present than ever before. I listened to a few of their presentations but most of the science is lost on me; there’s a lot in the pipeline, as they say. My big takeaway was we had more and better food at the conference than ever. Thank you Pharma!
I don’t believe so much in cures but I have a lot of hope for treatments. I have no regrets in life. having this condition has taught me things I likely never would have learned without it. my challenges have been many but I have found many ways to work around and mitigate the physical and emotional pain.
I do hope treatments are in the near future that can provide young families with more hope that their child can live a healthier and happier life. I know how devasted my mother was from the loss of an infant and she never lived to understand why.
Consider what you might be able to do for International Myotonic Dystrophy Awareness Day on September 15, 2023.